2022 Alzheimer’s Cure Breakthrough
It is estimated that nearly 5.8 million Americans are living with Alzheimer’s disease (AD). The majority of these individuals are over the age of 65. Experts indicate that this number is expected to double every 5-10 years and, by 2050, there will be close to 14 million individuals with the disorder. All the current treatments for AD are only for mild symptoms, including problems with reasoning and thinking, but not everyone responds to these medications. As well, these agents also have adverse effects that are not always tolerable. None of the currently available treatments have been shown to delay or prevent the progression of the disease. But, on the horizon, new studies are highlighting the way for more help to come.
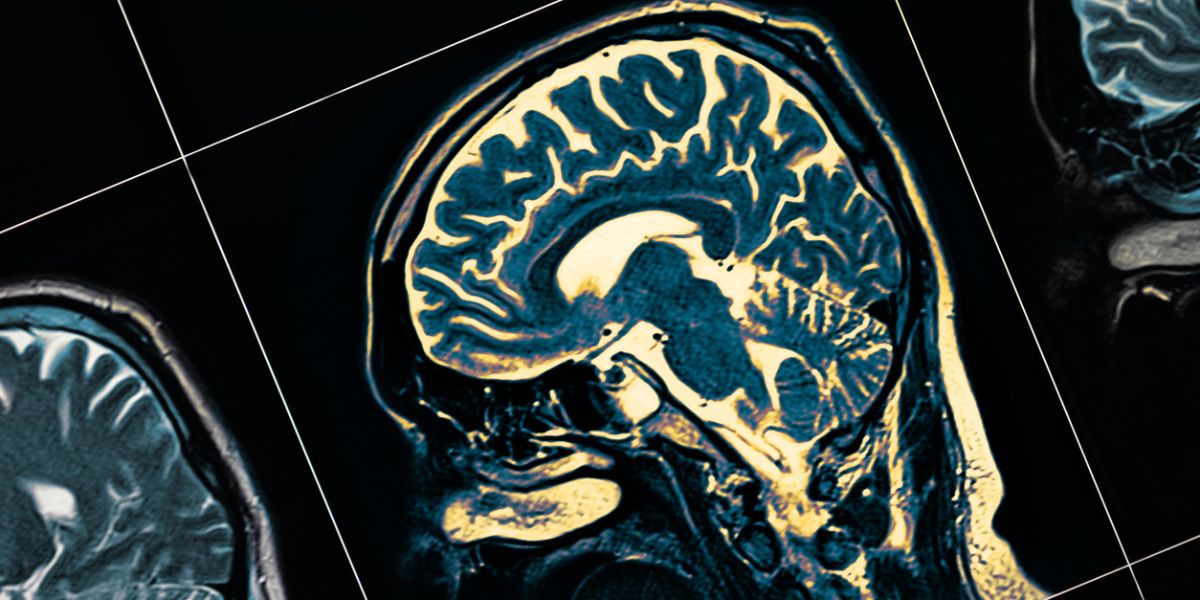
As the brain neurons die, the symptoms get worse, and the majority of AD individuals require admission to long-term care facilities as they become unmanageable at home. Over the past three decades, researchers have been trying to find treatments that can either delay or prevent AD. With a growing understanding of how AD affects the neurons in the brain, finally, there has been an Alzheimer’s cure breakthrough 2022. The majority of research has focused on the plaques in the brain of AD individuals. These plaques appear before the symptoms develop and if one could find a way to prevent the build-up of plaques, one can potentially prevent the symptoms from developing.
The New Treatments for AD
Alzheimer’s cure breakthrough studies and potential treatments have shown some promising results.
Dissolving the plaques: Most of the current focus on the management of AD has been targeting the protein plaques known as amyloid. These plaques are a classic feature of the disorder and often deposit early in the brain. Individuals who develop these plaques in the brain are more likely to develop symptoms of AD than those without plaques. Hence, several drugs (monoclonal antibodies) have been developed that prevent the formation or clumping of these amyloid plaques. The monoclonal antibodies are very similar to the naturally occurring antibodies in the blood circulation, but they have only one target: amyloid beta. Unfortunately, amyloid is not found in all patients with AD and why this happens is not known. It is believed that close to 30%-35% of AD patients with mild to moderate disease may not have brain amyloid and, hence, cannot benefit from this treatment.
Aducanumab: Last year, the US Food and Drug Administration approved Aducanumab, which is known as a monoclonal antibody, for the treatment of select cases of mild AD. This is the only approved drug in the US for the treatment of amyloid plaques in the brain. Once the plaques are removed, the brain cells stop dying, and the patient’s memory, thinking, function, and behavior stop worsening. However, there is still debate whether the drug actually works. While several small trials have shown that the drug not only prevents aggregation of amyloid but also decreases the symptoms, other clinical trials have shown no benefit. Plus, there are no long-term data on this agent yet and whether it can prevent dementia. However, there is hope for an Alzheimer’s cure breakthrough 2022.
Currently, Aducanumab is only approved for use in select patients with mild cognitive impairment or early Alzheimer’s disease. Before the treatment can be administered, all individuals with AD must undergo a PET scan to determine if they have amyloid plaques.
Several other monoclonal antibodies have also been developed (Gantenerumab, Lecanemab, and Donanemab) by different drug manufacturers and they also target amyloid in the brain. All these agents are currently being evaluated in clinical trials.
To be eligible for Aducanumab treatment, one has to meet the following criteria:
- Be less than age 85
- Have confirmed mild cognitive impairment
- Undergo a PET scan to determine the presence of amyloid plaques
- Have no recent history of a stroke or bleeding in the brain
- Not be on a blood-thinning medication
How is Aducanumab Administered?
To take the drug, you need an intravenous infusion every four weeks for as long as you live. This means going to a hospital or a clinic where an intravenous tube is inserted, and the monoclonal antibody is slowly infused over several hours. The other monoclonal antibody, Gantenerumab, can be administered below the skin, and one may be able to administer the drug at home; however, this technique does require some skill and supplies.
What are the Side effects of Aducanumab?
The most worrisome feature of Aducanumab are the side effects, which can include the following:
- Brain swelling that can cause headaches, change in mental status, vomiting, and difficulty walking
- Falls
- Diarrhea
- Confusion
All patients who receive Aducanumab have to be closely monitored by a team of doctors. If these side effects develop, the drug has to be immediately discontinued.
At the moment, more clinical trials are underway to determine its long-term side effects. Some insurers have declined coverage of Aducanumab and only a few centers in the USA are offering this therapy.
The Cost
Finally, it is important to know that this novel monoclonal antibody treatment for AD is very expensive. The cost of the drug is about $56K annually, or about $5,000 a month. Medicare has initiated a contract with the company so that the drug will be available for about $28K annually. There is also the additional cost of the PET scan ($5,000) and the administration of the drug; all totaled, the patient will be left with a hefty copayment.
Other Novel Treatments for AD
- Prevent destruction of the neurons. Other researchers have been focusing on treatment for AD that prevents destruction of the important neurons. The monoclonal antibody, Saracatinib, has been shown in animal studies to reverse memory loss and resume function of the neurons. The drug is currently being assessed in a small clinical trial.
- Prevent tangles: Other researchers are looking at drugs that can prevent the formation of tangles in the brain of AD individuals. A protein called a tau has been shown to form tangles in AD patients and this has been linked to dementia and behavioral problems. Currently, tau inhibitors and tau vaccines are being evaluated in clinical trials.
- Decreasing inflammation: Many scientists believe that in AD, the brain is in a state of low-level chronic inflammation, which continues to damage the nerves. Therefore, drugs are being developed that have an anti-inflammatory effect. Currently, the drug Sargramostim is being studied to determine if it can help AD patients.
Evaluating the Heart-to-Brain Connection
There is growing evidence indicating that the health of the brain is closely related to the health of the heart and blood vessels. Individuals who have damage to their blood vessels and heart tend to be at a higher risk for dementia. Thus, researchers are looking at the role of blood pressure control, diabetes, and cholesterol, and how they affect the brain. In general, it has been shown that people who have control of their blood pressure, diabetes, and cholesterol have a much lower risk of AD compared to those who have no control over these parameters. Today, many healthcare workers are encouraging patients to adopt a positive lifestyle that includes good nutrition, exercise, discontinuation of smoking, reduction of body weight, and limiting the intake of alcohol.
CONCLUSION
While researchers continue to develop new treatments for AD, it remains to be seen if they will prevent or reverse dementia. Plus, these new treatments could have less-than-desirable side effects. In the meantime, healthcare workers highly recommend adopting a positive lifestyle because early data show that it can delay or prevent the onset of dementia. Everyone is looking for an Alzheimer’s cure breakthrough 2022.
Cano Health is a patient-centered health services group that focuses on senior health care. They have instituted many programs to assist in keeping seniors healthy and active. Read the message from Dr. Marlow Hernandez Cano, D.O., M.P.H., M.B.A., F.A.C.P. here and call them at 1-855.975.5119 today to learn more about how they can help you. With everyone working together, there is hope for an Alzheimer’s cure breakthrough.